Background
Primary central nervous system lymphoma (PCNSL) is a rare and aggressive form of non-Hodgkin lymphoma. High-dose methotrexate is the cornerstone of treatment for PCNSL, often in combination with other agents. Outcomes are poor with an estimated 5-year overall survival (OS) of 30-40%. Outcomes in AIDS-related PCNSL have been historically inferior to immunocompetent individuals, although recent data suggests some improvement with anti-retroviral therapy. We sought to evaluate clinical characteristics, treatment patterns, and outcomes of patients with PCNSL at our institution.
Methods
A total of 30 patients were diagnosed and treated for PCNSL at Parkland Health and Hospital System (Dallas, TX) between 2010 and 2019. Parkland is a safety net hospital for Dallas County and is affiliated with the University of Texas Southwestern Medical Center. Electronic records were reviewed and data on demographics, clinical characteristics, treatment patterns, and outcomes were extracted. Descriptive statistics and survival data, comparing HIV(-) and HIV(+) patients, are presented.
Results
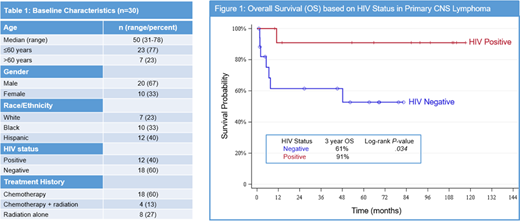
Median age at diagnosis was 51 years (range 24-78). Two thirds of patients were male and 40% (12 patients) were HIV(+). HIV(+) patients were younger compared to HIV(-) with a median age of 40 vs 57 years. Seventy three percent of patients belonged to minority groups (40% Hispanic; 33% Black). First line treatment consisted of chemotherapy in 18 (60%), chemotherapy and radiation in 4 (13%), and radiation alone in 8 (27%) patients; the latter was primarily used in HIV(+) patients (58%; 7/12). The most common chemotherapy regimen was CALGB 50202.HIV(+) patients were also started on anti-retroviral therapy. Fifty percent of the patients had a complete response (CR) to first line therapy. Five patients with a partial response converted to a CR with additional treatment for a final CR rate of 67%. CR rate was higher in HIV(+) patients. Five patients (17%), all HIV(-), experienced progression of disease while on 1st line treatment. Patients with progression of disease on treatment had poor response to salvage therapy and short survival (median OS 49 days). The majority of the patients were not eligible for autologous stem cell transplant (A-SCT) due to financial constraints or comorbid conditions. Only one patient underwent consolidation A-SCT, after achieving a second CR.
After a median follow up of 51 months, median OS was not reached. Three-year OS was 74% for the entire cohort. HIV(+) patients had a longer 3-yr OS compared to HIV(-) patients (91% vs 61%), this difference was statistically significant (p=0.034).
Conclusion
We report the outcome of PCNSL in a minority enriched population treated at a safety net hospital. Compared to prospective clinical trials, HIV(-) patients in our cohort had a lower than expected CR rate, although survival rates were comparable. In addition, we observed higher response rates and better overall survival in HIV(+) patients, including in those who were treated with combination of antiretroviral agents and radiation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal